Sub-Saharan Africa: mental health
This paper sets out to investigate mental health disorders in sub-Saharan Africa, and the extent to which they are influenced by various aspects of the government or state. Mental health disorders, in this context, are classed the mainstream way: depressive disorders, anxiety disorders, eating disorders, schizophrenia, and bipolar disorder; drug and alcohol use are included for purposes of comparison. The aim is to identify the extent to which government/state related variables predict mental health in sub-Saharan Africa. In other words, the aim is to obtain some indication of the extent to which government policies might help to “create” mental ill health in the population.
One might, from this perspective, understand mental health as consisting of two factors. The first of these is an innate predisposition to mental ill health that individuals might “carry with them”. These are theorised to be either genetic or socialised into individuals at a very young age. Factors such as a family history of mental ill health, as well as early adversity such as domestic abuse, bad parenting and bullying, among others, might play a role here.
The second major component consists of precipitating factors, which are external influences, or stressors. When paired alongside the predisposition, these can cause mental ill health to become manifest. This predisposition-threshold model is widely accepted within the discipline of psychology. The analysis seeks to identify some of the precipitating factors, rather than the prevalence of the innate aspects. If government policies or state bureaucracies have an impact on mental ill health, it is most obviously at this external point that they come to do so.
First, the prevalence of various categories of mental ill health is described. Secondly, those afflictions with the greatest prevalence were selected. Thirdly, these were correlated with contextual variables, to identify any government or state-related variables that influence mental ill health in the region.
The mental health data was obtained from various sources, including the Institute for Health Metrics and Evaluation (IHME), a research institute focusing on global health statistics at the University of Washington in Seattle.
The extent of mental ill health was measured in Disability Adjusted Life Years (DALYs). One DALY can be thought of as one lost year of healthy life. The sum of DALYs throughout the population can be thought of as the disease burden or the gap between actual disease situation and the ideal, where the population lives to an advanced age free of ill health. This is adapted from the WHO’s definition.
The external, government related variables were obtained from World Bank indicators and the United Nations Development Program (UNDP).
The IHME provides an indication of disease burden globally. Using their data, Richie and Roser (2019) created a series of visualisations of mental health and substance abuse disease burden. Their mappings are used in figures 1, 3 and 4. Considering figure 1, which maps global mental disorders and substance abuse, it appears that Africa is relatively devoid of these phenomena, and that these appear to be afflictions of the more advanced economies. Note, however, that the identification of psychological disorders is to an extent a western practice, and a number of arguments can be made about the validity of measuring western notions of mental health in an African context.
[Figure 1]
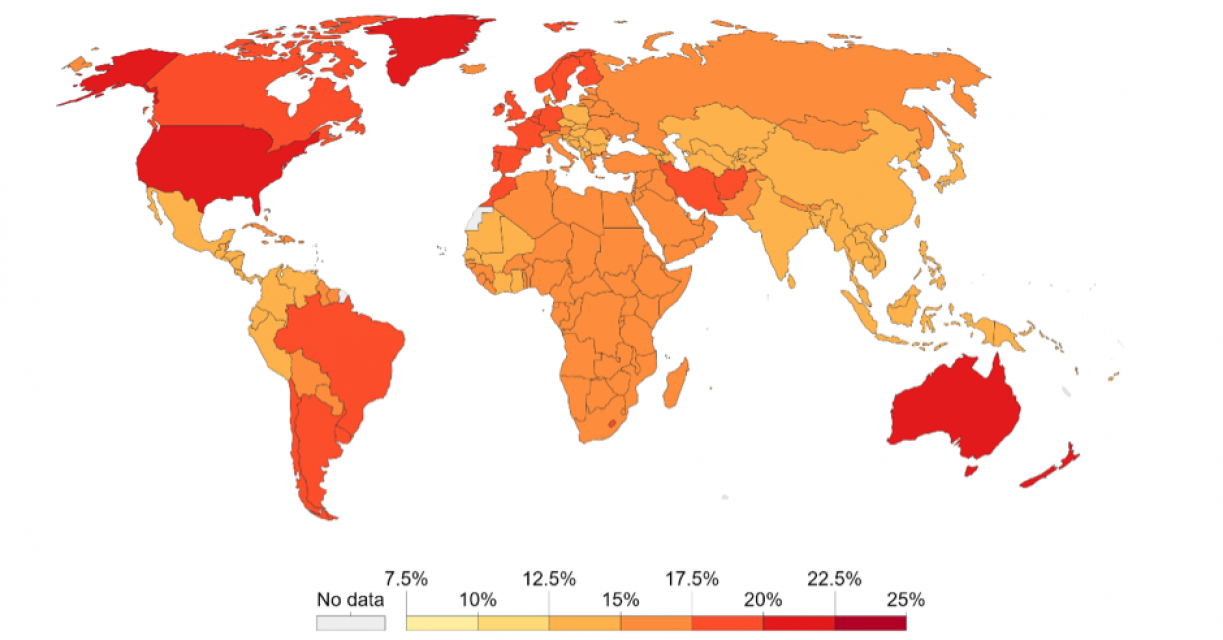
Figure 1: Global mental disorders and substance abuse (from Richie and Roser, 2019)
If we break mental ill health in sub-Saharan Africa down into its constituent afflictions, the prevalence of mental health issues in that region shows a high degree of variation.
[Figure 2]
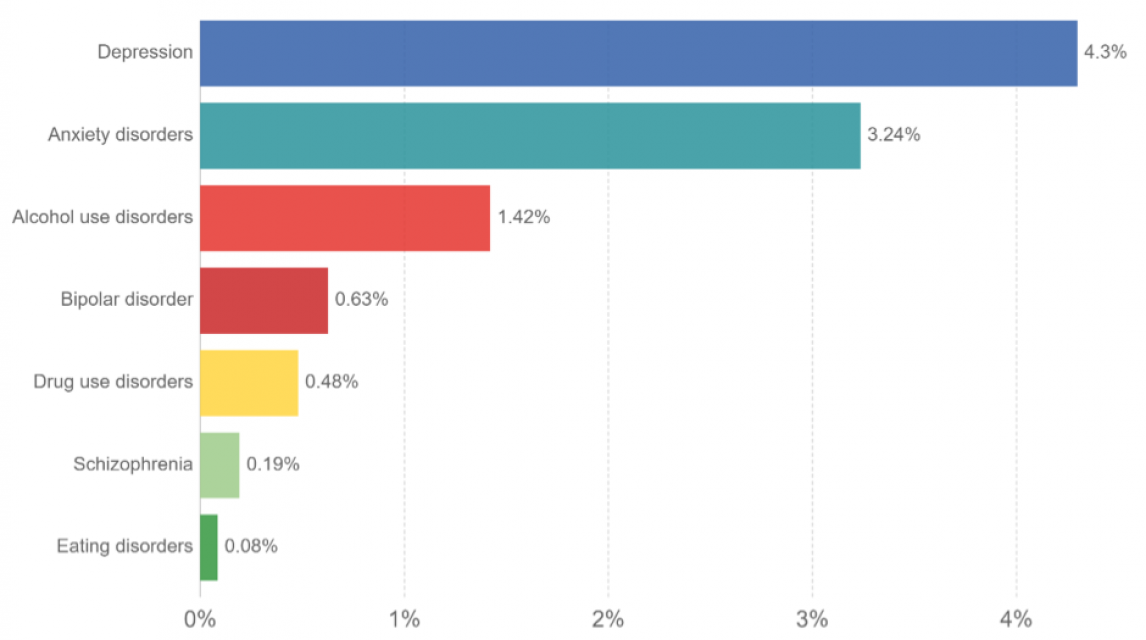
Figure 2: Various classes of mental disorder in sub-Saharan Africa
It is evident that depressive and anxiety disorders are the major mental health challenges in this region. The IHME displays this graphically:
[Figure 3]
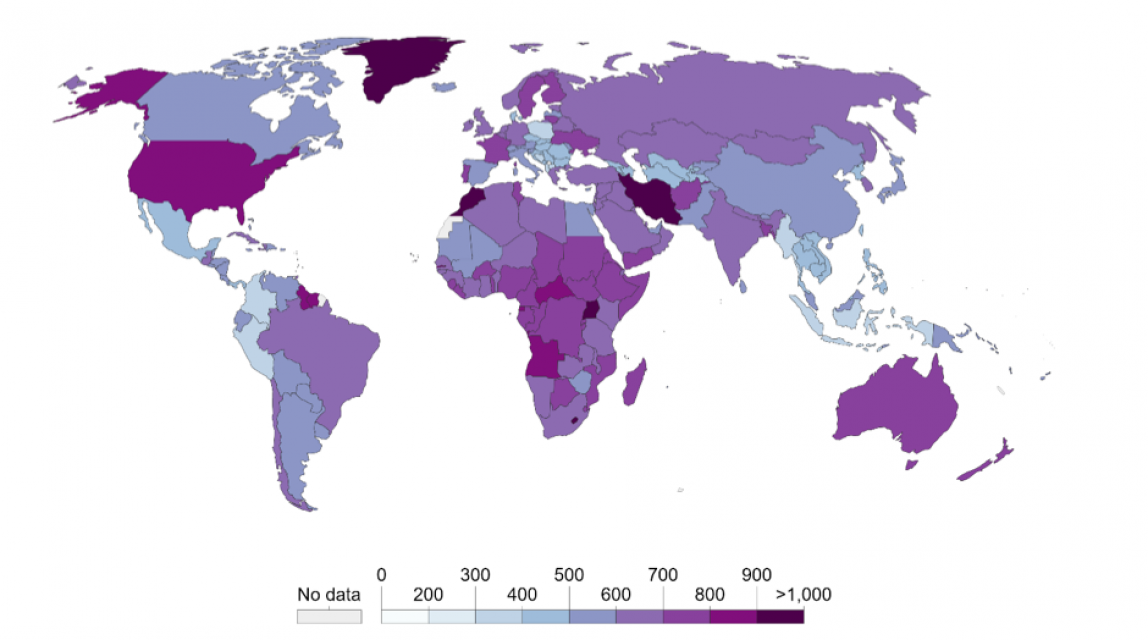
Figure 3: Global depressive disorders (from Richie and Roser, 2019)
The prevalence of depressive disorders in Africa is heterogeneous, and is closer to the severe end of the spectrum, globally. The heterogeneity suggests some complexity to the aetiology of depression throughout the region. Anxiety is far less prevalent across the region.
[Figure 4]
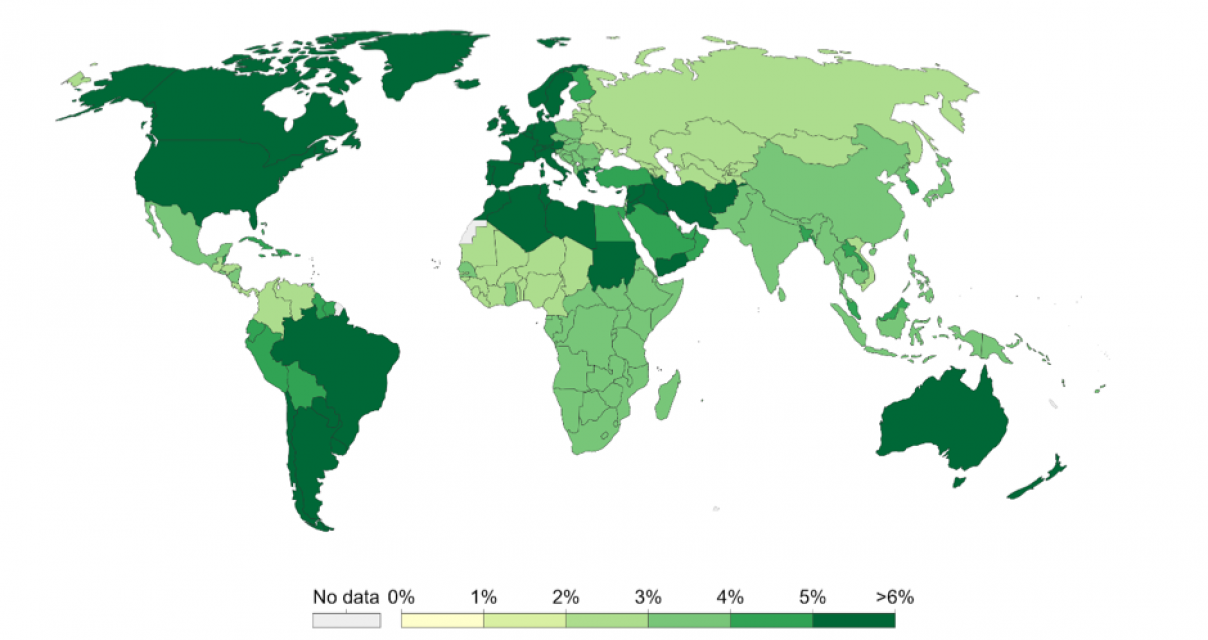
Figure 4: Global anxiety disorders (from Richie and Roser, 2019)
The question is: to what extent these patterns can be explained by factors at least partially under government control or as related to states’ service provision?
The following graph illustrates the risk factors associated with depressive and anxiety disorders. It is evident that problems in family dynamics account for a large portion of depressive aetiology – a pattern seen uniformly across the world. Of course, these family dynamics are very likely caused by contextual factors themselves. In the following sections, the analysis will move beyond these immediate family/household–related factors. As mentioned, we want to focus on the factors that push people over the threshold into mental ill health. This puts the focus onto the contextual stressors rather than on innate and biological factors or early life socialisation (such as bullying and childhood maltreatment).
[Figure 5]
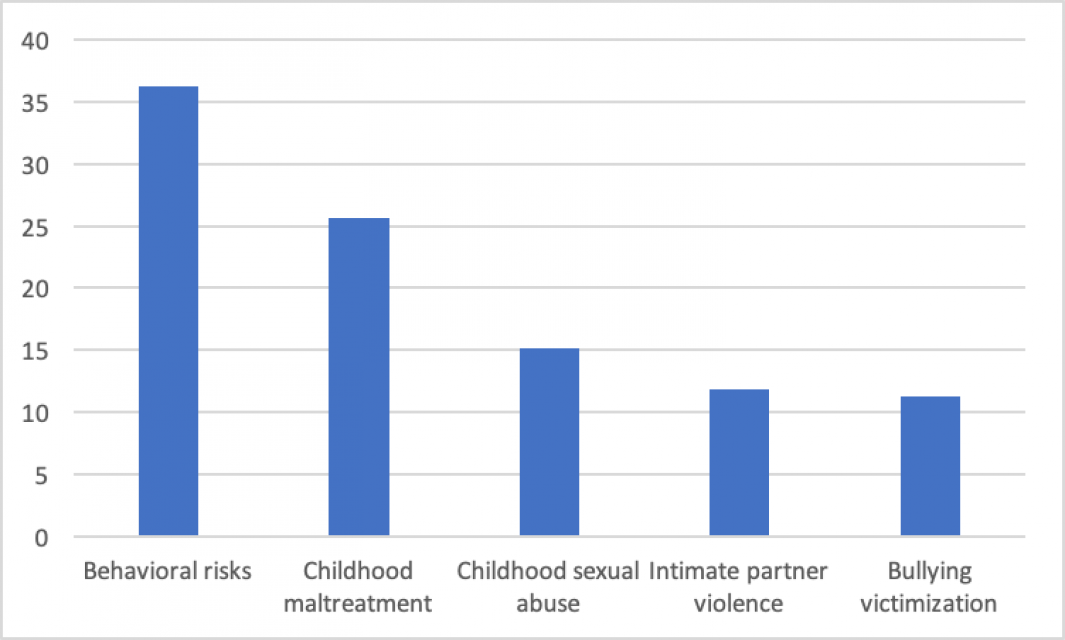
Figure 5: Risk factors associated with depressive disorders in sub-Saharan Africa (from IHME data)
There is some indication in the literature of the broader contextual factors that might predispose individuals to depressive episodes. The most obvious of these are income and education. Both of these variables have been shown to have some relevance to depression globally. These are therefore included in the analysis.
But this analysis goes further by investigating additional variables obtained from World Bank data. These include air pollution, access to basic services, migration and refugees, rural-to-urban shifts, gender equality and government expenditure on health. The choice of which variables to include in the analysis was constrained, to a large degree, by the available data. It was hypothesised, however, that all of these contextual factors would have some impact on the prevalence of depression and/ or anxiety disorders in the country.
In order to do so, a correlation matrix was created for the variables in question. Ideally, a multiple regression would have been used, but the available data precluded this. From this, the most influential external factors were selected. In our analysis, only the rural urban shift proved to have a measurable impact on depression, alongside income and education.
The government/state factor was included in the analysis in the way that the measures were constructed. While services were not found to be clearly related to depression, investment in education was found to be related. The significant outcomes were plotted on a graph, which also reflected gender differences.
[Figure 6]
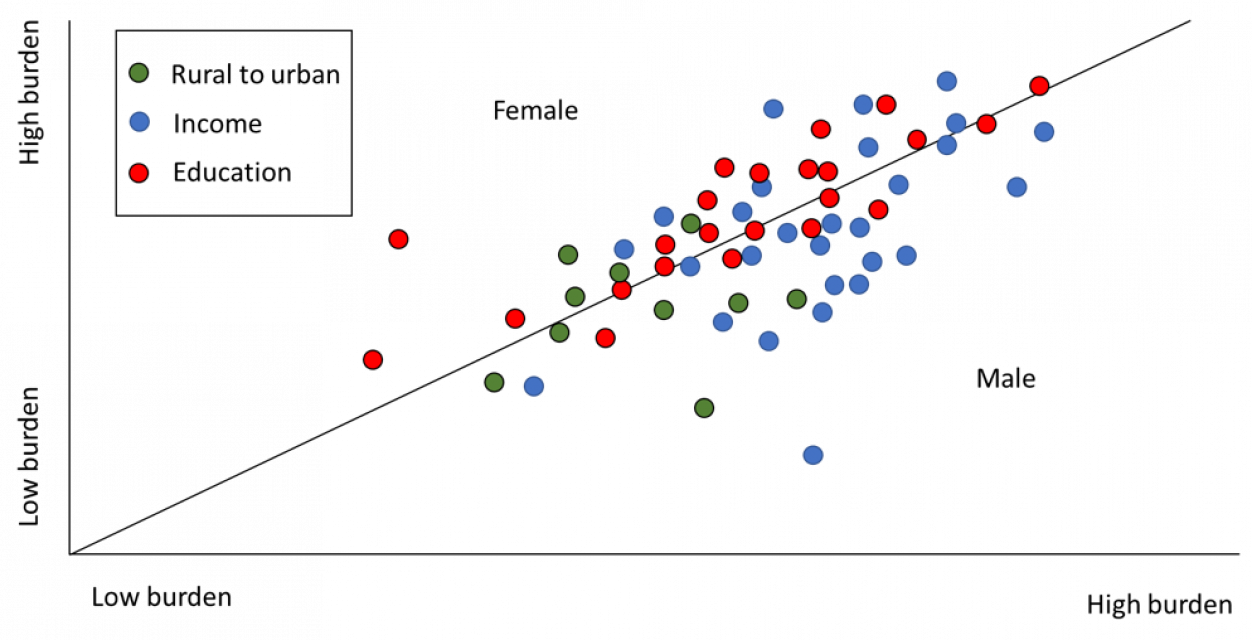
Figure 6: Education, income and rural-to-urban migration as related to depressive disorders in sub-Saharan Africa.
Figure 6 presents data for three stressors: education, income and rural-to-urban migration when related to depressive disorders, measured in number of DALYs lost. Each dot represents a sub-Saharan country, broken down by gender (DALYs lost by females and DALYs lost by males in that country). The position of the dot is then determined by the coordinates of the female and male score. The vertical line indicates the switch from female to male bias in the impact of depression.
The graph, therefore, allows one to see gender bias in depression burden by noting whether the dot falls above or below the vertical line. It also allows for an understanding of the severity of the burden. Dots further towards the top right represent higher burdens. Not all sub-Saharan countries are plotted – only those in which depression could be reliably linked to the stressors in the analysis were included. Also, the names of the countries were not included. Although this would be an interesting addition, it was felt that this might detract from the overall message/pattern in the data. For a similar reason, a broad indication of the severity of the burden was included on the x and y axes, rather than the exact DALY burden.
It is evident from the graph that there is some variation in the influence of gender, depending on the predisposing factor. Education is seen to be more of a factor for females than for males. This effect was found to be of moderate strength. Income, on the other hand, was found to be more influential for male depression. The third factor – rural-to-urban migration – did not display a noticeable effect between gender, and was less influential overall
These findings suggest that government investment in education has an unintended consequence of boosting mental health within the population.
The same methodology was applied to anxiety disorders. As with the depressive disorders, a correlation matrix was constructed for the variables in question. Once again, from this, the most influential external factors were selected and included in the analysis. Only one variable emerged, alongside education and income. This was access to services. To preserve some comparability, the rural-urban shift was also included in the plot.
[Figure 7]
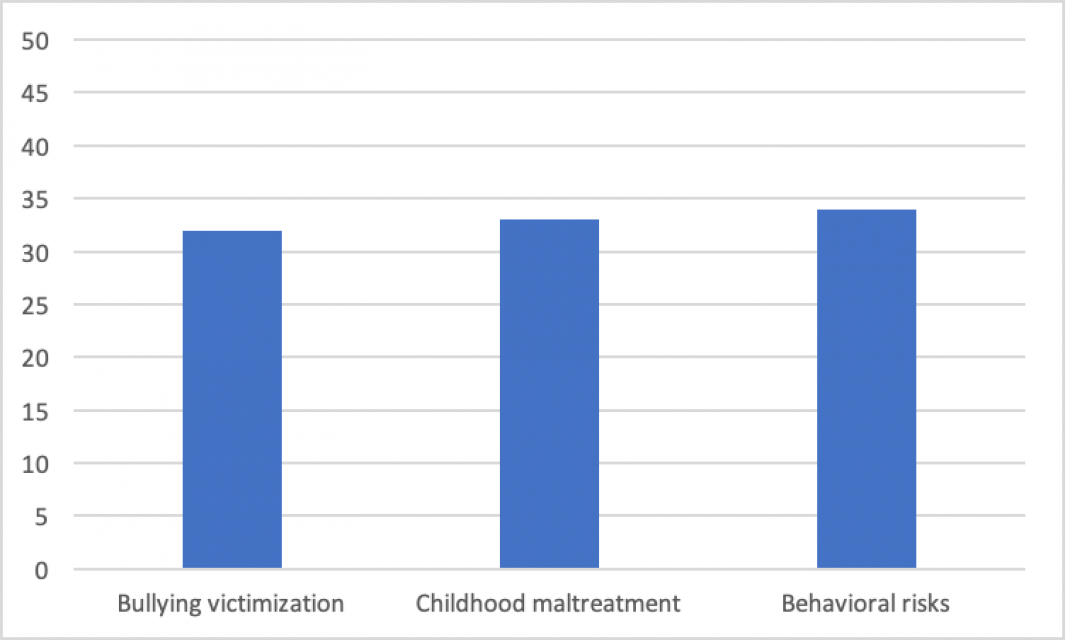
Figure 7: Traditional, family and household factors as related to anxiety disorders in sub-Saharan Africa.
From this graph it is evident that there is no single overarching causal factor regarding anxiety disorders. Is it possible, however, that broader socio-political issues also have an impact on the high anxiety disorder burden in sub-Saharan Africa? To gain some idea of this, a number of contextual factors were investigated; air pollution, access to basic services, migration and refugees, rural-to-urban shifts, gender equality and government expenditure on health.
[Figure 8]
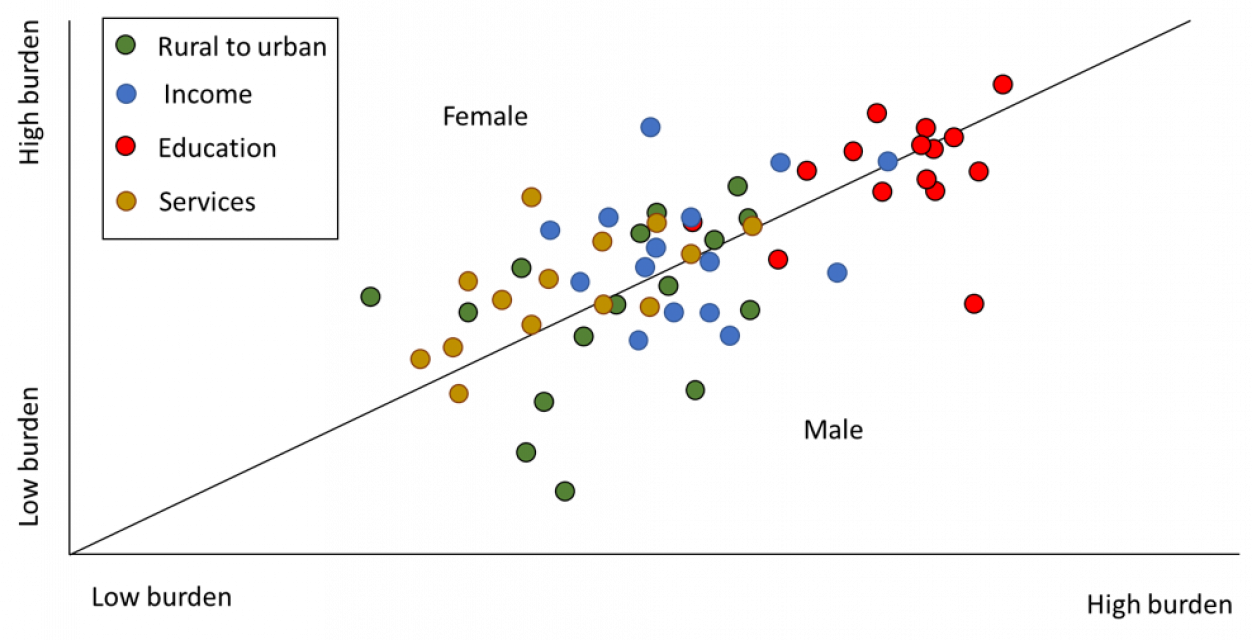
Figure 8: Education, income, rural-to-urban migration and services as related to anxiety disorders in sub-Saharan Africa.
In the case of anxiety disorders, investment in education was clearly more influential than the other factors. In addition, there seemed to be less of a gender bias in this effect, with no noticeable difference being exhibited between females and males. Income showed no clear correlation with anxiety, and neither did rural-to-urban migration. Services, however, showed a noticeable effect on anxiety disorders. The services scale included factors such as access to sanitation and the provision of safe drinking water. It is worth noting, however, that the services included in the analysis were not exhaustive; rather, they were constrained by the available data. Anxiety related to access to services showed a noticeable bias towards females.
Figure 9
Figure 9: Education, income, rural-to-urban migration and services as related to depressive and anxiety disorders in sub-Saharan Africa.
It is possible, merely by superimposing the depressive and anxiety graphs, to observe the combined effect of the four variables that came out as significant. When combined, the gender biases are less obvious, except in the case of services – which is unsurprising, since services appeared as significant in anxiety disorders only. The other variables show very little bias.
The analysis suggests that Africa is not as badly affected by mental health issues as more westernised/industrialised countries. Although the terminology is difficult, it might be said that this state of affairs may be expected to change as Africa moves more in line with globalisation. Depression and anxiety are, currently, the major disorders regarding mental ill health. These disorders have a large social component – as opposed to a condition like schizophrenia, which appears to be more biologically/genetically based.
The IHME data indicated that the risk factors associated with these two classes of disorder are largely family/household related, and include factors such as having an abusive partner or being bullied, among others. Beyond these factors – which are typical of global mental ill health aetiology – the broader context was found to have some impact on the expression of these disorders. Income and education – the latter was measured via government-related variables, such as investment in education, among others – were found to be related to both depression and anxiety, although in different ways. This suggests that mental health is affected by the environment in which individuals find themselves.
More importantly, these mental disorders are to a significant part affected by the diligence of government. The state’s underinvestment in education and services, and the failure to protect a basic level of income has a noticeable impact on their citizens’ levels of depression and anxiety.
This is a bold claim, and it opens up some questions for future research and clarification. Most obvious is the suitability of the data collected. Critics of mainstream psychology have noted that these disorders emerged from a western, industrialised context. Some powerful critiques have questioned the extent to which these are valid concepts in an African context. One might suggest that the more industrialised/westernised/globalised Africa becomes, the less the importance that should be attached to this question. The problem of whether these are appropriate constructs, however, remains. Future research might be directed toward this issue.
Another area for further investigation relates to the issue of how these issues should be addressed. A strong critique of psychology has been that it offers no effective cure for the ills that it describes. Typically, psychotherapy has been seen as the remedy to psychological problems. The effectiveness of psychotherapy has been questioned, but the real problem with psychotherapy probably has more to do with the fact that it is slow and typically expensive.
It seems unlikely, at least for the foreseeable future, that Africa’s mental health challenges will be addressed by armies of psychotherapists working at affordable rates. How, then, should these issues be tackled? One way is by conducting this kind of investigation into the uniquely African predisposing factors, and then addressing these factors via activism or some other means. Considered from this perspective, the most important message of this brief exploration is that a much more thorough investigation of the contextual and state-related predisposing factors to mental ill health needs to be carried out.